Discharge Planning is Broken: Why Independent Patient Advocates Are the Missing Link Patients Desperately Need

Discharge Planning is Broken: Why Healthcare Advocates Are the Missing Link Patients Desperately Need
What You'll Learn in This Article
Discharge planning is meant to help patients transition safely from hospital to home—but all too often, it fails. In this article, you’ll learn why most discharge plans fall short, how that failure puts patients and families at risk, and what a better discharge process should actually include. You’ll also explore practical solutions that family caregivers and professionals can act on immediately to reduce stress and improve outcomes. Whether you’ve experienced a rushed discharge firsthand or you work in healthcare, this piece will give you insight—and a path forward.
The Real Problem with Discharge Planning
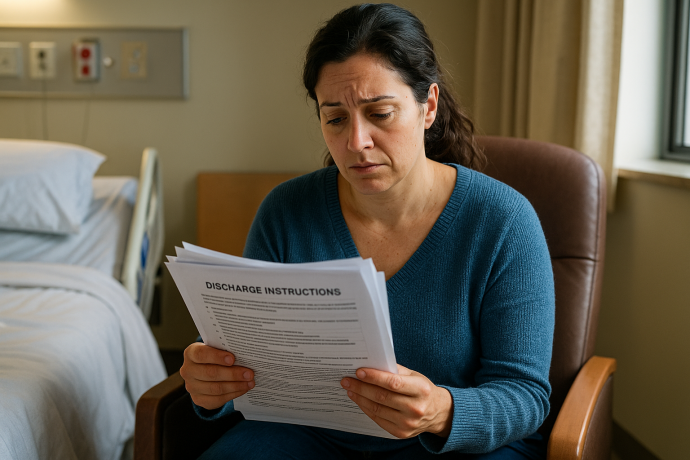
Safe hospital discharge processes are supposed to thoughtful, planned transition meant to help patients transition safely from the hospital to home or the next level of care. But in practice? It’s often a checklist dumped on an already overwhelmed caregiver, handed out 15 minutes before transport arrives. That means:
- No walkthrough of what “home care” really means.
- No real-world plan for managing meds, follow-ups, equipment, or red flags.
- No confirmation or coordination between what medical equipment was ordered and what actually shows up at home
- No emotional or logistical support for the caregiver absorbing it all.
That's not safe discharge planning. That's discharge scrambling. But I know firsthand that it hasn't always been this way. I was a Social Work discharge planner at a Level 1 Trauma Center. Back then, discharge planning meant preparing the family, equipping the home, and collaborating across disciplines (PT, OT, and Chaplains are some of my favs). Now? I'm horrified at how low the bar has fallen. What's often labeled «discharge planning» today wouldn't have passed as a bare minimum in the past.
Why it Matters and Who Pays the Price
Poor discharge planning isn’t just inconvenient. It’s dangerous and expensive.
- 1 in 5 Medicare patients are readmitted within 30 days.
- Missed meds, skipped follow-ups, or confusion about care plans are major causes of hospital readmissions.
- Untrained family caregivers are routinely expected to perform medical tasks (like wound care or injections) with no family caregiver training or support.
The costs of poor discharge planning are devastating: physical harm, caregiver burnout, fractured family dynamics, and rising healthcare costs. That bill is paid with stress, loss of sleep, missed work, and disruption of family life.
What Better Discharge Planning Could Look Like
An Independent Patient Advocate can make a critical difference.
Better discharge planning isn't a form or a phone number, it's a system of support. Independent Patient Advocates work with families to help build that system.
Here’s what patient-focused, goal-aligned discharge planning should include:
- A real conversation about the patient and family goals, life, and expectations—not just a handout
- Family caregiver training on medical tasks they'll be expected to perform
- A check-in within 48 hours of discharge to troubleshoot breakdowns
- A single point of contact to coordinate across doctors, facilities, and vendors
- A plan grounded in realistic expectations, not idealized assumptions
The Role of Independent Patient Advocates
When hospitals and facilities fall short, Independent Patient Advocates step in. Here's what advocates across the country are already doing:
- Attending discharge planning meetings and asking the right questions
- Hitting «pause» on unsafe discharge plans
- Listening to the goals and realities of the patient and family, and overlaying a safe discharge plan on that
- Ensuring durable medical equipment (DME) is delivered, installed, and explained
- Creating medication reconciliation lists and verifying pharmacy fulfillment
- Coordinating follow-up appointments and transportation
- Providing family caregivers with written guides and one-on-one coaching
- Troubleshooting insurance issues, including prior authorizations and coverage questions
- Tracking warning signs that could lead to readmission
Advocates help families feel less alone and more in control during one of the most stressful transitions in healthcare. We can do that because Independent Patient Advocates work for the patient—not the hospital, facility, or insurance company.
Private, Independent Patient Advocacy is the Bridge
Discharge planning, as it stands, is broken. But Independent Patient Advocates are the bridge between the chaos of the hospital or facility and the continuity of home care. We fill the gaps, speak up when families don't know how, and help reduce the risk of readmission and harm.
Whether you're a family caregiver, a concerned friend, the patient, or a hospital-based professional, know this: you don't have to navigate it alone.
We work for you.
We want the best for you—whatever your best might look like.
We are ready to walk this road with you.