To Vent or Not To Vent: Re-Examining Advance Directives
COVID-19 is rapidly changing the medical landscape in the United States and throughout the world. For many people who already have advance care directives in place, these rapid changes should signal an important opportunity to review their plans. Decisions made pre-COVID-19 don’t take into account the challenging specifics of this disease. Being proactive and considering how this pandemic may impact advance care directives can save everyone time, money, and help prevent unnecessary suffering.
(For more information on Covid-19 advocacy, check out this blog on changes to advocacy techniques or this blog on talking to patients.)
«I believe everyone should examine their end-of-life wishes and take the reality of the current pandemic into account… If you chose to forgo ventilator assistance, it may be beneficial to consider adding it.»
The Basics About Advance Directives:
An advance care directive is a legal document that details the health-related measures for prolonging life you would like to be undertaken if you aren’t able to make decisions for yourself. You can also designate a medical power of attorney (POA) to make health-related decisions if you can’t speak for yourself. Advance directives cover various life-prolonging and comfort-care measures such as the use of life-prolonging equipment, do not resuscitate (DNR) orders, artificial hydration and/or nutrition, and the administration of comfort care measures such as medicine to relieve pain, anxiety, and nausea. Although these directives are an important document at any time, they are especially critical in the current health landscape as COVID-19 can strike unexpectedly and critical illness can occur rapidly.
What Directives Look Like Across the Country:
Approximately one in three Americans have an advance care directive. But many of these people have not made updates to their documents in light of COVID-19. I believe everyone should examine their end-of-life wishes and take the reality of the current pandemic into account when doing so. For those who had previously chosen to forgo ventilator assistance, it may be beneficial to consider adding a short-term ventilator plan. And for those who have chosen to receive full treatment under other circumstances, it is useful to consider whether they still want to receive full treatment, including ventilation, if diagnosed with COVID-19. To start thinking about this, let’s take a look at what we know about ventilators and COVID-19.
About Mechanical Ventilation:
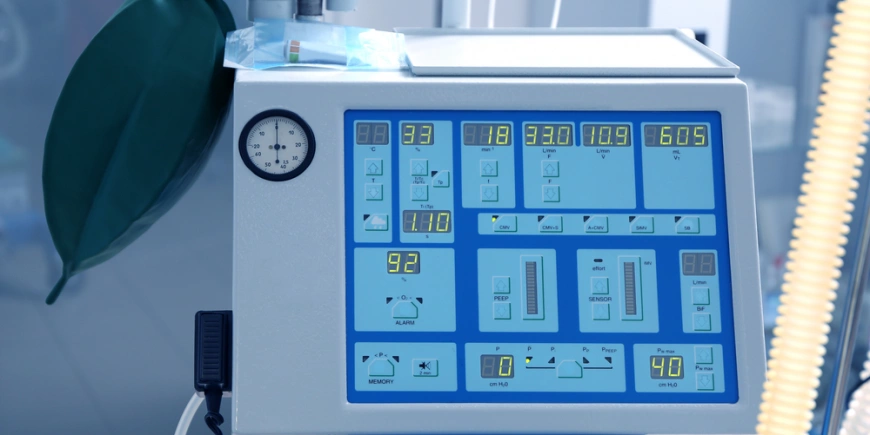
Mechanical ventilation is one tactic being used on critically ill COVID-19 patients due to severe respiratory symptoms. Mechanical ventilators are machines which help you breathe. You can be intubated, that means a tube goes down your throat, or you can receive a “trach”. A “trach” is a tube that is inserted through a hole in the neck. COVID-19 patients who decide to be ventilated typically remain on ventilation for 2–3 weeks. Long-term ventilation like this can cause severe lung disease and some patients may ultimately take months to recover. Most importantly, a ventilator is not a cure for COVID-19, it simply allows your body the time it may need to recover. Of patients in New York City who were intubated, 24.5% eventually passed away.
Ventilation Pros and Cons:
When considering and discussing your advance care plan in light of COVID-19, it is important to weigh the pros and cons of ventilation. Because COVID-19 can strike unexpectedly and develop into a severe illness rapidly, patients who do not have plans in place may not have the time to develop them. Many hospitals have no-visitor policies, so the chance to discuss medical decisions with loved ones is limited. And for patients who are on ventilation, speaking is no longer possible.
My Personal Thoughts About Ventilation:
I am a board-certified patient advocate, and just a few days ago, I was considering my own advance care directive. Before the rise of COVID-19, my advance care directive stated I did not want to be placed on a ventilator. However, in light of the current pandemic, should I add a short-term ventilator plan? Maybe. At the very least, I should consider how COVID-19 may impact my wishes.I always attempt to be proactive instead of reactive. This is especially valuable to keep in mind when it comes to COVID-19.
Having the Ventilation/Directive Discussion:
Conversations about these preferences and values can help provide real relief for the patient and their loved ones. There’s comfort in having a plan in place in times like these. I’ve also included a list of resources at the end of the article to help you think about updating your advance care directive due to COVID-19 or to put an advance care directive into place for the first time if you don’t currently have one. Having these difficult planning conversations now can save individuals pain and suffering due to unwanted medical procedures and save their families from undue emotional and financial hardship.
Other topics to consider during these discussions include:
Your feelings about being put on and taken off a ventilator.
How to handle a curable condition that is currently life-threatening.
The appointment of a medical power of attorney (POA) who you trust to make medical decisions based on your values and wishes.
How to get information on the available types of treatment.
Although our medical landscape looks different today than it did just a few months ago, you can ensure you are prepared for any eventuality by thinking about your advance care directive in light of COVID-19 and making any changes that are needed now. Remember, it pays to be proactive instead of reactive. Don’t wait to think about and make these important changes.
(For more information on the future of Covid-19, check out this blog )
It’s important to have your voice heard when decisions are being made for you.f
1https://www.reuters.com/article/us-health-usa-advance-directives/over-one-third-of-u-s-adults-have-advanced-medical-directives-idUSKBN19W2NO
2https://www.reuters.com/article/us-health-coronavirus-ventilators-specia/special-report-as-virus-advances-doctors-rethink-rush-to-ventilate-idUSKCN2251PE
3 www.medpagetoday.com/infectiousdisease/covid19/86101
Advance Directive Resources:
Luckily, there are lots of resources available to help you have these talks and assist you in thinking about the best decisions for you and your individual situation. Remember, an advance care directive shouldn’t be “just a piece of paper.” It should be the embodiment of a larger conversation where you consider what is most important to you such as loved ones, mobility, and independence.
The National Hospice and Palliative Care Organization provides links to each state’s advance directive form.
The Conversation Project offers three concrete steps you can take now to begin thinking about your wishes during the current pandemic. There are also helpful conversation prompts to assist you while having these difficult conversations.
theconversationproject.org/wp-content/uploads/2020/04/tcpcovid19guide.pdf
Five Wishes provides many resources to support you and your loved ones in discussing and documenting end-of-life care and comfort choices.
Fivewishes.org
Respecting Choices has several COVID-19 planning and discussion tools, including information on specific treatment decisions and the importance of making treatment decisions before a medical crisis.
respectingchoices.org/covid-19-resources/
Compassion and Choices offers a comprehensive end-of-life planning guide in Spanish and English. They also have a useful COVID-19 specific addendum which can be completed to add to your advance care directive. This addendum includes additional specificity to address the possible progression of COVID-19.
compassionandchoices.org/resource/covid-19-advance-care-planning/
